Tumors Hijack the Nervous System to Fuel Their Own Growth
www.scientificamerican.com
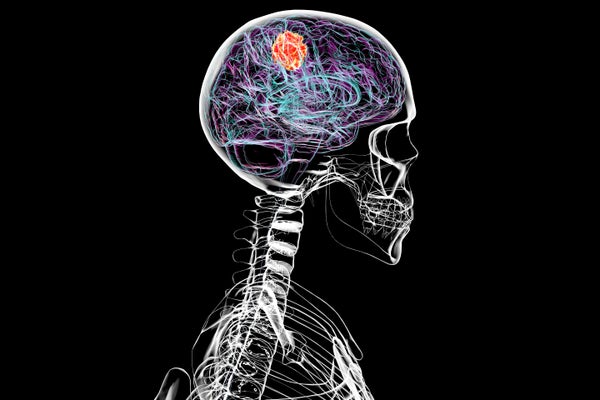
February 14, 20259 min readTumors Hijack the Nervous System to Fuel Their Own GrowthInterrupting signals exchanged between tumors and the nervous system could become a critical pillar of cancer careBy Ingrid Wickelgren edited by Gary StixBrain tumor. Kateryna Kon/Science Photo Library/Getty ImagesCancer arises as an enemy from within. One of the bodys own cells becomes damaged or corrupted and then multiplies to create copies of its aberrant self. The ballooning army of deviant cells may invade nearby tissues, damaging them and causing symptoms.Deepening the betrayal, the body itself becomes complicit. Blood vessels grow toward the tumor, supplying oxygen and nutrients. Immune cells may forego an attack on the cancer and protect it instead. By communicating with these body systems, the cancer bends them to its own ends.Until recently, the nervous system was not thought to be part of these duplicities, even when cancer had set up its primary residence in the brain. Neurons were simply the cancers victims. But in recent years, investigators have uncovered chemical and electrical cross talk between neurons and cancer cells that powerfully fuel a tumors growth. The tumor may even remodel neural networks so that they are better positioned to provide it critical life support.On supporting science journalismIf you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.The discoveries unveiling this alliance underpin a new field called cancer neurosciencethe study of interactions between cancer and the nervous system that promote cancer growth and cancer-related disability.Michelle Monje, a neuroscientist and neuro-oncologist at Stanford University, helped pioneer the field more than a decade ago while studying a group of deadly brain cancers that include glioblastoma and certain fatal childhood tumors. The strongest evidence for the devastating actions of the nervous system in cancer is in brain cancermuch of it a result of Monjes work. But researchers have replicated at least part of the story in other cancers, including those of the breast, prostate, pancreas, colon and skin.The findings offer a new set of targets for halting cancer growth. Monje believes that interrupting the communication between cancer and the nervous system may be key to successfully treating the deadliest of tumors.Scientific American spoke to Monje about the strategies neurons and cancer cells use to collaborate and the ways that drugs might be crafted or repurposed to disrupt that relationship.[An edited transcript of the interview follows.]How did cancer neuroscience get its start?Its only been about 10 years, and it really came all at once. My intellectual journey started during my clinical training, between 2000 and 2010. I was treating patients with primary brain cancers called high-grade gliomas, for which we have extremely limited therapies. Youve probably heard of glioblastoma [a type of high-grade glioma]. I also focus on a childhood cancer called diffuse midline glioma. It struck me that these cancers happen in particular parts of the nervous system at particular ages. You can predict the location of a glioma if you know the age of the patient. That speaks to some process in neural development that has gone awry.I also knew that for almost 100 years, neuropathologists looking at tumor tissue have noticed cancer cells clustering around neurons in the brain. The cells are not randomly distributed. They have this tight microanatomical association with mature neurons that we call perineuronal satellitosis.What did you make of those clues?I thought the cancer might be hijacking neurodevelopment. As a neuroscientist, I knew that much of neurodevelopment depends on the activity in the nervous system. So I thought the activity of the nervous system might matter a lot in brain cancer. There might be critically important interactions between the neurons and the cancer cells.Was that a new idea?Yes. At that time, neurons had been entirely ignored [as participants in cancer]. They were viewed solely as the victims of the cancer.How did you test this idea?We put tumors that had been removed from my patients into mouse brains. Then we used a technique called optogenetics, which allows us to control the activity of specific neurons, to stimulate mouse neurons. We found that the tumors grew more and that they grew faster. It was the first demonstration that brain activity influences brain cancer growth.In that same study, which was published in 2015, we also identified some growth factors that the active neurons secrete that influence the growth of the glioma.You said this happened all at once. What other evidence had come out?Around that time, a very exciting paper from the sadly now deceased Paul Frenette, who was working at Albert Einstein College of Medicine, showed that peripheral nerves were important for prostate cancer growth. Then a third group led by Tim Wang at Columbia [University] showed that if you remove nerves in the stomach in a mouse model of gastric cancer, the tumors stop growing.A program officer at the National Cancer Institute [NCI] took notice of our work and suggested we have a think-tank meeting. In 2015 she brought us all together at the NCI for what was really the very first meeting in cancer neuroscience.So nervous system activity causes the release of chemical factors that spur cancer growth. Is that the whole story?Not all of what we were seeing in my lab could be explained by these growth factors. As a postdoc, I had discovered that these terrible childhood high-grade gliomas originated from immature cells that give rise to oligodendrocytes, brain cells that belong to a broad class called glia. In my lab, we showed that neural activity causes normal immature glia to mature and proliferate and that it does so through growth factors. We found that one of these factors, a surprising one called neuroligin 3, strongly regulates the growth of malignant glioma. In fact, it was required for glioma growth: if you deleted the gene for it in a mouse, gliomas from patients did not grow in the mouses brain.We delved into why the cancer was dependent on this factor, and we found that when glioma cells were exposed to it, they expressed genes that are needed for building synapses [the connection points between neurons]. So I wondered whether synapses might be forming between neurons and the cancerwhich seemed like a really wild idea. But we looked, and there were.So the cancer cells are electrically connected to neurons in a circuit?We not only found neuron-to-cancer synapses but also electrical currents in the cancer cell. This cancer is an electrically active tissue. We can see it. We have a biochemical tool that shows us the electrical activity. The electrical potential difference across the cell membrane changes, something called membrane depolarization [that lets positively charged ions stream into the cell]. Thats a super metabolically expensive thing for a cell to do, so it must be advantageous to the cancer cell.I wondered whether this membrane depolarization was the key thing. The synapses were important because they induce membrane depolarization. We tested that by using optogenetics to depolarize cancer cells in a mouse brain, and that did promote the cancers growth. So just membrane depolarization is sufficient to promote the growth of the cancer.We showed that in a paper published in 2019. Then, in 2023, we reported that the larger the inward current, the more it promotes the growth of the cancer. And if we interrupt this current, that is pretty profoundly therapeutic in animal models.Were you the first to find these synapses between the cancer and the nervous system?Back in December 2015, when we were still working on proving this, I was invited to speak at [Heidelberg University in Germany] by Frank Winkler, who had just discovered that glioma cells connect to each other through something called gap junctions. We were talking in this office, and although I had just met this guy, I decided to share our really big finding.... His face lit up. He said, We found synapses, too!It was so incredibly reassuring. It wasnt some artifact. This independent group across the Atlantic found the exact same thing. In a lot of contexts, people would be competitive about this co-discovery. But I wasnt going to try to scoop him, and he didnt try to scoop me. Instead we co-submitted our papers to Nature. They were published back-to-back in the same 2019 issue. Its a nice story of scientific professionalism.When the cancer cells form these synapses, does the brains normal activity promote their growth?Yes, and the cancer cells even remodel the brain. A neurosurgeon colleague of mine, Shawn Hervey-Jumper of the University of California, San Francisco, made some chilling discoveries in adults who had been newly diagnosed with gliomas that affected the left language cortex. Prior to removing the tumors, he recorded from the region around the tumor while patients did expressive language tasks, such as naming objects in photographs. In people without tumors, the expressive language centers become active during these kinds of tasks. But in these patients, a much larger area spanning the entirety of the tumor-infiltrated cortex became active. So by the time of diagnosis, the tumor had functionally remodeled language circuitry such that every time a patient spoke, the tumor was stimulated.How did the tumor do this?Cancer cells secrete factors that lead to more neuron-to-neuron synapses and increase excitability and probably promote this functional remodeling, which we only partly understand.Does that mean that, using these factors, the cancer recruits and mobilizes the nervous system to further promote its own growth?Yes, the remodeling creates more connections to the tumor such that normal activities, such as speaking, trigger more extensive electrical inputs to the tumor than they would otherwise. The tumor also increases the activity of neurons so there are more instances of communication between the neuron and the cancer.Its a vicious cycle. [This remodeling of circuitry not only perpetuates the cancers growth but also] probably accounts for a lot of the symptoms patients have. Hervey-Jumper found that language function in patients inversely correlated with the degree to which the cancer had remodeled the language circuitry. Survival was also inversely correlated with the degree to which the tumor was connected to the rest of the brain.Is this a new idea?Yes. Most people thought these neurological deficits resulted from a destructive process, and thats not true. Theres a dysfunction process induced by the cancer and hijacking of the neural circuits, but the cancer needs the neural circuits to function, so destruction is much more minimal and much later in the course of the disease.Does the nervous system play a role in all cancers?In every solid tumor Im aware of that has been studied from this perspective, there is a key neural mechanism that is regulating cancer initiation, growth and/or invasion. But there are a lot of cancers that have not been studied from this perspective.Are these mechanisms the same as they are for brain cancer?Peripheral nerves are important for peripheral cancers. So the concept is the same, but the details differ from tumor to tumor. For instance, cholinergic nerves [which release a chemical signal called acetylcholine] powerfully drive colon cancer, but those same nerves slow down pancreatic cancer, which is driven by adrenergic nerves [which release adrenaline].People have found neurotransmitters and growth factors driving the growth of these cancers, but we dont know as much about synaptic and electrical mechanisms in cancers outside of the brain because those experiments are just beginning to be done.What are the implications for cancer treatment?There are key opportunities to develop new and repurpose old medicines to target these neuron-cancer interactions. We are starting in this field with a leg up because so many wonderful medicinesfor seizures, migraines, blood pressure and arrhythmias, for examplehave already been developed that target neurotransmitter receptors and ion channels to regulate excitable tissues. In our 2019 paper, we tested an antiseizure medicine called perampanel that targets a receptor on glioma cells. It really nicely slowed glioma growth in mice. We can take FDA-approved medicines off the shelf and test them in this new way.There are also lessons to be learned from data we already have. A lot of cancer patients take antiseizure medicines, blood pressure medicines and pain medicines. We can study patient datasets to see if people did better if they were on one of these other medications.Are there clinical trials?The trials are just beginning. I led an early-phase trial of a compound that blocks the release of neuroligin 3 in pediatric brain tumors. Frank Winkler has started a glioblastoma trial targeting neurotransmitter receptors and gap junctions that are involved in signaling between neurons and cancer cells. There are trials of beta-blockers in breast cancer.Do you think that disrupting nerve-cancer interactions will be enough to control cancer?Probably not. But I suspect it will be necessary for difficult-to-treat cancers. As somebody who administers CAR T cell therapy [genetic modification of a patients immune cells] for brain tumors, I can tell you that one of the reasons that this immunotherapy doesnt work sufficiently is that these are rapidly growing tumors, and the treatment cant keep up. It is hard to get ahead of the cancer. But if you can disconnect the tumor from the nervous system that is robustly promoting its growth, maybe you can slow it down enough to allow the immunotherapy to outpace the cancer.Treatments based on this idea will not replace current cancer treatment strategies, such as chemotherapy, surgery and radiation. They will augment them to increase their efficacy and hopefully achieve better outcomes. Targeting nervous system interactions with cancer is going to be a major aspect of cancer care in the future.What does the future look like for cancer neuroscience?The field has been exploding. We just had a cancer neuroscience meeting in January with 125 attendees, a 10-fold increase from that first meeting a decade ago. And there are so many papers that every time I write a review article, it feels out of date by the time it is published.We are developing courses in cancer biology for the neuroscientist and in neuroscience for the cancer biologist. We need to teach each other the techniques because there are very few of us trained in both disciplines. We are also training the next generation of scientists to learn neuroscience and cancer biology techniques at the same time. Its so exciting that people are thinking about this now. Its really this missing pillar of oncology.
0 Commentarios
·0 Acciones
·84 Views