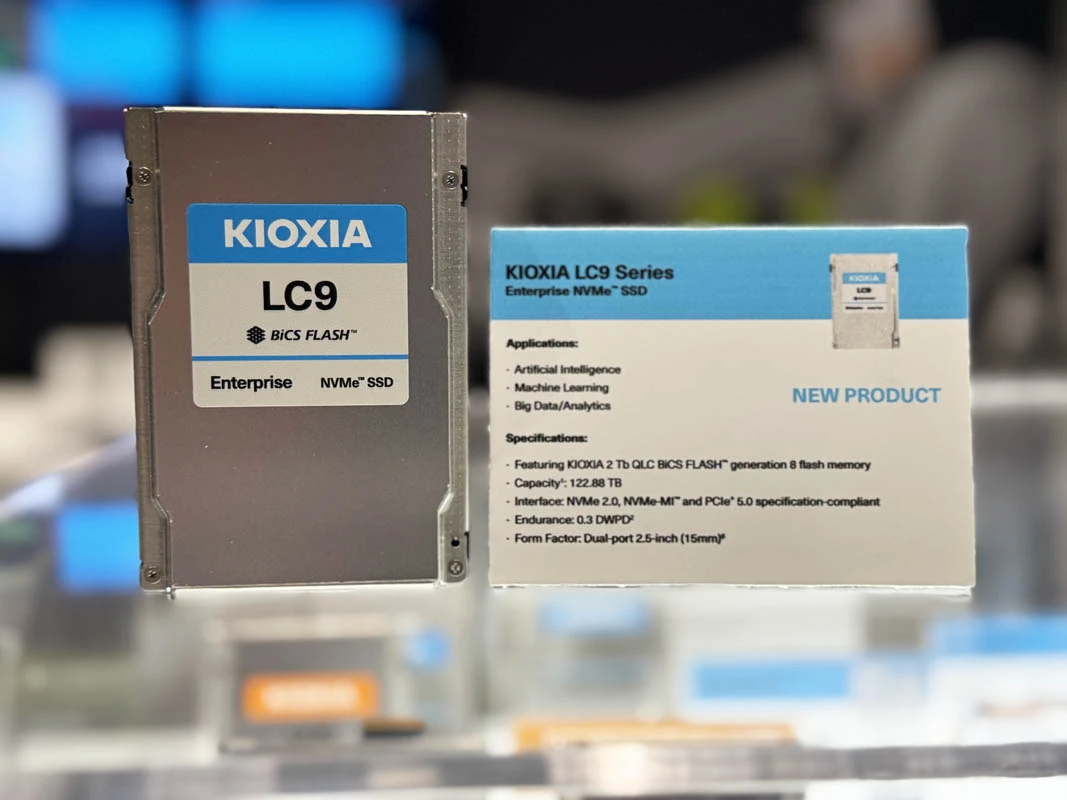
Kioxia launched a new SSD with a capacity of 245 terabytes. That's a lot of storage, I guess. It might be useful for someone, but honestly, I’m not too excited about it. Just another day, another launch.
#Kioxia #SSD #245TB #Storage #TechNews
#Kioxia #SSD #245TB #Storage #TechNews
Kioxia launched a new SSD with a capacity of 245 terabytes. That's a lot of storage, I guess. It might be useful for someone, but honestly, I’m not too excited about it. Just another day, another launch.
#Kioxia #SSD #245TB #Storage #TechNews