0 Σχόλια
0 Μοιράστηκε
174 Views

Κατάλογος
Κατάλογος
-
Παρακαλούμε συνδέσου στην Κοινότητά μας για να δηλώσεις τι σου αρέσει, να σχολιάσεις και να μοιραστείς με τους φίλους σου!
-
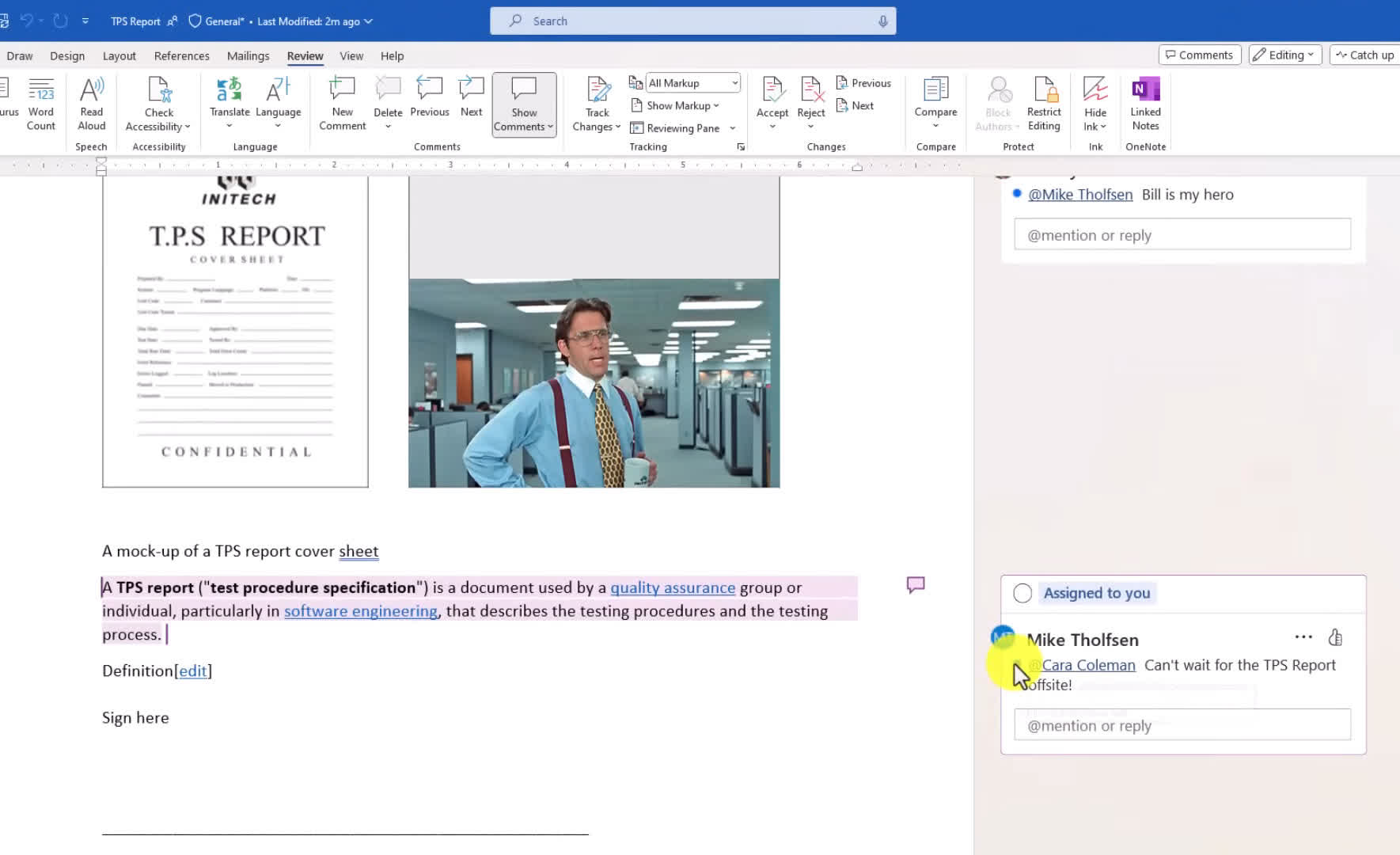 WWW.TECHSPOT.COMUnlock your productivity with Office 2024: new features and a lifetime dealMicrosoft Office has long been the cornerstone of productivity for professionals and students alike. Office 2024 is the latest version of the suite, bringing an overall design refresh to align with modern aesthetics, offering a more intuitive user experience across all applications.For a limited time, you can buy a lifetime license for Microsoft Office 2024 Home & Business for PC or Mac at a reduced price of $159, down from the regular price of $249.99. This one-time purchase grants lifetime access to essential applications, including Word, Excel, PowerPoint, Outlook, and OneNote, without the need for recurring subscription fees.What's New in Office 2024?Word 2024 offers new tools to help you craft engaging content, featuring Document Recovery, compatibility with ODF 1.4, and a convenient option to remove all resolved comments in one step. New collaboration tools have been incorporated so multiple users can share a document, leave comments, or ask questions directly in the document, easily toggle between Viewing, Reviewing, and Editing modes, and clear all resolved comments with a single click.Transferring images from your phone to your PC used to be a multi-step process, but with Office 2024, you can now seamlessly insert photos directly from your Android device into your documents.Enjoy enhanced performance in Excel 2024. The integration of dynamic arrays allows for more flexible data manipulation, enabling users to create formulas that return multiple values and automatically adjust to accommodate new data entries. Furthermore, Excel introduces new text and array functions for complex data operations.PowerPoint 2024 introduces several practical new tools. You can now record your presentation capturing your voice, ink annotations, and even your video presence, then save it as a shareable video file. Additionally, you can enhance accessibility by adding closed captions to video and audio content.Find what you need more easily in Outlook 2024 with improved search capabilities, offering more accurate results for emails, files, contacts, and events.Lifetime license and other detailsOffice 2024 retains much of the familiarity of Office 2021 but introduces a refreshed default theme inspired by Windows 11's Fluent Design principles. The suite also debuts a new default font, Aptos, replacing Calibri for a modernized look.Microsoft is calling Office 2024 their latest "locked-in-time" update to Word, Excel, PowerPoint, and other applications, designed for users who prefer not to use the continuously evolving Microsoft 365 versions (which cost you subscription money). Microsoft will provide official support for Office 2024, including bug fixes and security updates for five years, until October 9, 2029.This offer provides immediate delivery of your license key and download, making it super convenient and granting you instant access to the software.StackSocial is a trusted partner of TechSpot, managing the TechSpot Store reliably for over a decade. Prices are subject to change.Here's a summary of other current Microsoft software deals:Windows 11 Pro available for $18Microsoft Visual Studio Professional for $34Microsoft Office 2019 Pro Plus available for $27Microsoft Office 2021 Pro available for $69Microsoft Project 2021 for Windows for $18Microsoft Visio 2021 for Windows for $180 Σχόλια 0 Μοιράστηκε 171 Views
WWW.TECHSPOT.COMUnlock your productivity with Office 2024: new features and a lifetime dealMicrosoft Office has long been the cornerstone of productivity for professionals and students alike. Office 2024 is the latest version of the suite, bringing an overall design refresh to align with modern aesthetics, offering a more intuitive user experience across all applications.For a limited time, you can buy a lifetime license for Microsoft Office 2024 Home & Business for PC or Mac at a reduced price of $159, down from the regular price of $249.99. This one-time purchase grants lifetime access to essential applications, including Word, Excel, PowerPoint, Outlook, and OneNote, without the need for recurring subscription fees.What's New in Office 2024?Word 2024 offers new tools to help you craft engaging content, featuring Document Recovery, compatibility with ODF 1.4, and a convenient option to remove all resolved comments in one step. New collaboration tools have been incorporated so multiple users can share a document, leave comments, or ask questions directly in the document, easily toggle between Viewing, Reviewing, and Editing modes, and clear all resolved comments with a single click.Transferring images from your phone to your PC used to be a multi-step process, but with Office 2024, you can now seamlessly insert photos directly from your Android device into your documents.Enjoy enhanced performance in Excel 2024. The integration of dynamic arrays allows for more flexible data manipulation, enabling users to create formulas that return multiple values and automatically adjust to accommodate new data entries. Furthermore, Excel introduces new text and array functions for complex data operations.PowerPoint 2024 introduces several practical new tools. You can now record your presentation capturing your voice, ink annotations, and even your video presence, then save it as a shareable video file. Additionally, you can enhance accessibility by adding closed captions to video and audio content.Find what you need more easily in Outlook 2024 with improved search capabilities, offering more accurate results for emails, files, contacts, and events.Lifetime license and other detailsOffice 2024 retains much of the familiarity of Office 2021 but introduces a refreshed default theme inspired by Windows 11's Fluent Design principles. The suite also debuts a new default font, Aptos, replacing Calibri for a modernized look.Microsoft is calling Office 2024 their latest "locked-in-time" update to Word, Excel, PowerPoint, and other applications, designed for users who prefer not to use the continuously evolving Microsoft 365 versions (which cost you subscription money). Microsoft will provide official support for Office 2024, including bug fixes and security updates for five years, until October 9, 2029.This offer provides immediate delivery of your license key and download, making it super convenient and granting you instant access to the software.StackSocial is a trusted partner of TechSpot, managing the TechSpot Store reliably for over a decade. Prices are subject to change.Here's a summary of other current Microsoft software deals:Windows 11 Pro available for $18Microsoft Visual Studio Professional for $34Microsoft Office 2019 Pro Plus available for $27Microsoft Office 2021 Pro available for $69Microsoft Project 2021 for Windows for $18Microsoft Visio 2021 for Windows for $180 Σχόλια 0 Μοιράστηκε 171 Views -
 WWW.DIGITALTRENDS.COMSpaceX shares photos of Starship ahead of sixth flight on TuesdaySpaceX is just a couple of days away from sending its enormous Starship rocket on its sixth test flight from its facility in Boca Chica, Texas.The mission had originally targeted Monday, November 18, for the launch of the vehicle comprising the main-stage Super Heavy booster and the upper-stage Starship spacecraft but on Friday SpaceX pushed the launch to Tuesday, November 19. Heres how to watch a live stream of the mission.Recommended VideosThe Elon Musk-led spaceflight company has just released a set of images (below) showing the 120-meter-tall Starship stacked and pretty much ready to fly.RelatedPropellant load test and preflight checkouts complete ahead of Starships sixth flight test, SpaceX said in a post on X.Propellant load test and preflight checkouts complete ahead of Starship's sixth flight test https://t.co/oIFc3u9laE pic.twitter.com/r6XNKyY2Zf SpaceX (@SpaceX) November 17, 2024The Starship took its first test flight in April 2023, but it only lasted a matter of minutes before an anomaly prompted the mission team to blow up the rocket in midair over the Gulf of Mexico.But each subsequent flight showed improvements in every aspect of the rockets performance. On the fifth flight last month, SpaceX performed a successful and truly spectacular catch of the 70-meter-tall Super Heavy at its first attempt, a challenging maneuver that took place as the booster returned to Earth following its deployment of the Starship spacecraft to orbit.Packing a colossal 17 million pounds of thrust at launch, the Starship is the most powerful rocket ever to get off the ground. Once fully tested, NASA and SpaceX want to use the vehicle to transport crew and cargo to the moon, Mars, and possibly beyond. It could even be configured to fly around 100 people in a single flight, though a mission of that magnitude is a long ways off.One of the Starships first big tests will be to use a modified version of the upper-stage spacecraft to land two NASA astronauts on the lunar surface in the Artemis III mission, which is currently scheduled for 2026.Editors Recommendations0 Σχόλια 0 Μοιράστηκε 175 Views
WWW.DIGITALTRENDS.COMSpaceX shares photos of Starship ahead of sixth flight on TuesdaySpaceX is just a couple of days away from sending its enormous Starship rocket on its sixth test flight from its facility in Boca Chica, Texas.The mission had originally targeted Monday, November 18, for the launch of the vehicle comprising the main-stage Super Heavy booster and the upper-stage Starship spacecraft but on Friday SpaceX pushed the launch to Tuesday, November 19. Heres how to watch a live stream of the mission.Recommended VideosThe Elon Musk-led spaceflight company has just released a set of images (below) showing the 120-meter-tall Starship stacked and pretty much ready to fly.RelatedPropellant load test and preflight checkouts complete ahead of Starships sixth flight test, SpaceX said in a post on X.Propellant load test and preflight checkouts complete ahead of Starship's sixth flight test https://t.co/oIFc3u9laE pic.twitter.com/r6XNKyY2Zf SpaceX (@SpaceX) November 17, 2024The Starship took its first test flight in April 2023, but it only lasted a matter of minutes before an anomaly prompted the mission team to blow up the rocket in midair over the Gulf of Mexico.But each subsequent flight showed improvements in every aspect of the rockets performance. On the fifth flight last month, SpaceX performed a successful and truly spectacular catch of the 70-meter-tall Super Heavy at its first attempt, a challenging maneuver that took place as the booster returned to Earth following its deployment of the Starship spacecraft to orbit.Packing a colossal 17 million pounds of thrust at launch, the Starship is the most powerful rocket ever to get off the ground. Once fully tested, NASA and SpaceX want to use the vehicle to transport crew and cargo to the moon, Mars, and possibly beyond. It could even be configured to fly around 100 people in a single flight, though a mission of that magnitude is a long ways off.One of the Starships first big tests will be to use a modified version of the upper-stage spacecraft to land two NASA astronauts on the lunar surface in the Artemis III mission, which is currently scheduled for 2026.Editors Recommendations0 Σχόλια 0 Μοιράστηκε 175 Views -
 WWW.DIGITALTRENDS.COMWatch Yellowstone season 5, episode 10: release date, time, channel, and plotAfter an almost a two-year hiatus, the Dutton family finally returned to prime-time television with Yellowstoneseason 5, part 2.Even with the time off,Yellowstoneremained a ratings juggernaut, as the premiere generated a whopping 16.4 million viewers across all cable networks and CBS airings. Thats an increase of 3% from the season 5, part 1 premiere, which registered 15.9 million viewers.Recommended VideosThis Season on Yellowstone | Paramount NetworkThe next episode ofYellowstone season 5, episode 10 premieres at 8 p.m. ET/PT on Sunday, November 17. The episode will air on Paramount Network.Watch Yellowstone on Paramount NetworkRelatedYellowstoneairs on Paramount Network, not Paramount+. Paramount Network is a cable channel that can be accessed through your TV package orParamount Networks website. You will need to log in with a TV provider for access. Unlike last week, a replay ofYellowstonewill not air on CBS.Paramount Network is available on several live streaming TV services, includingHulu with Live TV, Fubo, Philo, and YouTube TV. These services offer popular channels without having to pay for a cable box. Plus, several of the services offer free trials, so you could theoretically watch tonights episode at no cost.Paramount NetworkYellowstonemight be a Paramount show, but its not on Paramount+. Due to a previous licensing agreement, Yellowstonestreams on Peacock. However, Peacock subscribers cannot stream Yellowstoneseason 5, episode 10 tonight. The current season must air on Paramount Network before heading to Peacock. It could take a few months after the finale before theseYellowstoneepisodes live on Peacock.Emerson Miller / Paramount NetworkThe Yellowstoneseason 5, episode 10 is titled The Apocalypse of Change. Paramount Networks logline for the episode reads: Beth comes to a chilling realization. Kayce reaches out to an old friend in search of information. Jamie meets with Market Equities.ParamountIn the season 5, part 2 premiere, Beth (Kelly Reilly) and Kayce (Luke Grimes) head to their fathers mansion. Much to their shock, they learn John has died. The siblings find Johns body in the bathroom with a pistol nearby, leading the authorities to deem his death a suicide. Beth is suspicious right away and believes Jamie (Wes Bentley) is responsible for her fathers death.Beth doesnt believe her father committed suicide. Her feelings are confirmed later in the episode. Jamies fixer girlfriend, Sarah Atwood (Dawn Olivieri), is the one who orchestrated Johns murder. Sarah told the hit men to make Johns death look like a suicide.The Paramount NetworkWillYellowstoneseason 5, part 2 be the end of the Dutton family? With Costner gone,Yellowstone ending after season 5, part 2 seemed like a foregone conclusion. However, after the premieres record-breaking ratings, it seems like Yellowstonecan clearly continue without Costner, and it might end up doing so. Reilly and Cole Hauserhave been in talks for a potential sixth season. At this point, its all up to Sheridan.Watch Yellowstone on Paramount NetworkWhen youre done here, check out the best new shows to stream this week, as well as the best shows on Netflix, the best shows on Hulu, the best new shows on Max, the best shows on Amazon Prime Video, and the best shows on Disney+.Editors Recommendations0 Σχόλια 0 Μοιράστηκε 186 Views
WWW.DIGITALTRENDS.COMWatch Yellowstone season 5, episode 10: release date, time, channel, and plotAfter an almost a two-year hiatus, the Dutton family finally returned to prime-time television with Yellowstoneseason 5, part 2.Even with the time off,Yellowstoneremained a ratings juggernaut, as the premiere generated a whopping 16.4 million viewers across all cable networks and CBS airings. Thats an increase of 3% from the season 5, part 1 premiere, which registered 15.9 million viewers.Recommended VideosThis Season on Yellowstone | Paramount NetworkThe next episode ofYellowstone season 5, episode 10 premieres at 8 p.m. ET/PT on Sunday, November 17. The episode will air on Paramount Network.Watch Yellowstone on Paramount NetworkRelatedYellowstoneairs on Paramount Network, not Paramount+. Paramount Network is a cable channel that can be accessed through your TV package orParamount Networks website. You will need to log in with a TV provider for access. Unlike last week, a replay ofYellowstonewill not air on CBS.Paramount Network is available on several live streaming TV services, includingHulu with Live TV, Fubo, Philo, and YouTube TV. These services offer popular channels without having to pay for a cable box. Plus, several of the services offer free trials, so you could theoretically watch tonights episode at no cost.Paramount NetworkYellowstonemight be a Paramount show, but its not on Paramount+. Due to a previous licensing agreement, Yellowstonestreams on Peacock. However, Peacock subscribers cannot stream Yellowstoneseason 5, episode 10 tonight. The current season must air on Paramount Network before heading to Peacock. It could take a few months after the finale before theseYellowstoneepisodes live on Peacock.Emerson Miller / Paramount NetworkThe Yellowstoneseason 5, episode 10 is titled The Apocalypse of Change. Paramount Networks logline for the episode reads: Beth comes to a chilling realization. Kayce reaches out to an old friend in search of information. Jamie meets with Market Equities.ParamountIn the season 5, part 2 premiere, Beth (Kelly Reilly) and Kayce (Luke Grimes) head to their fathers mansion. Much to their shock, they learn John has died. The siblings find Johns body in the bathroom with a pistol nearby, leading the authorities to deem his death a suicide. Beth is suspicious right away and believes Jamie (Wes Bentley) is responsible for her fathers death.Beth doesnt believe her father committed suicide. Her feelings are confirmed later in the episode. Jamies fixer girlfriend, Sarah Atwood (Dawn Olivieri), is the one who orchestrated Johns murder. Sarah told the hit men to make Johns death look like a suicide.The Paramount NetworkWillYellowstoneseason 5, part 2 be the end of the Dutton family? With Costner gone,Yellowstone ending after season 5, part 2 seemed like a foregone conclusion. However, after the premieres record-breaking ratings, it seems like Yellowstonecan clearly continue without Costner, and it might end up doing so. Reilly and Cole Hauserhave been in talks for a potential sixth season. At this point, its all up to Sheridan.Watch Yellowstone on Paramount NetworkWhen youre done here, check out the best new shows to stream this week, as well as the best shows on Netflix, the best shows on Hulu, the best new shows on Max, the best shows on Amazon Prime Video, and the best shows on Disney+.Editors Recommendations0 Σχόλια 0 Μοιράστηκε 186 Views -
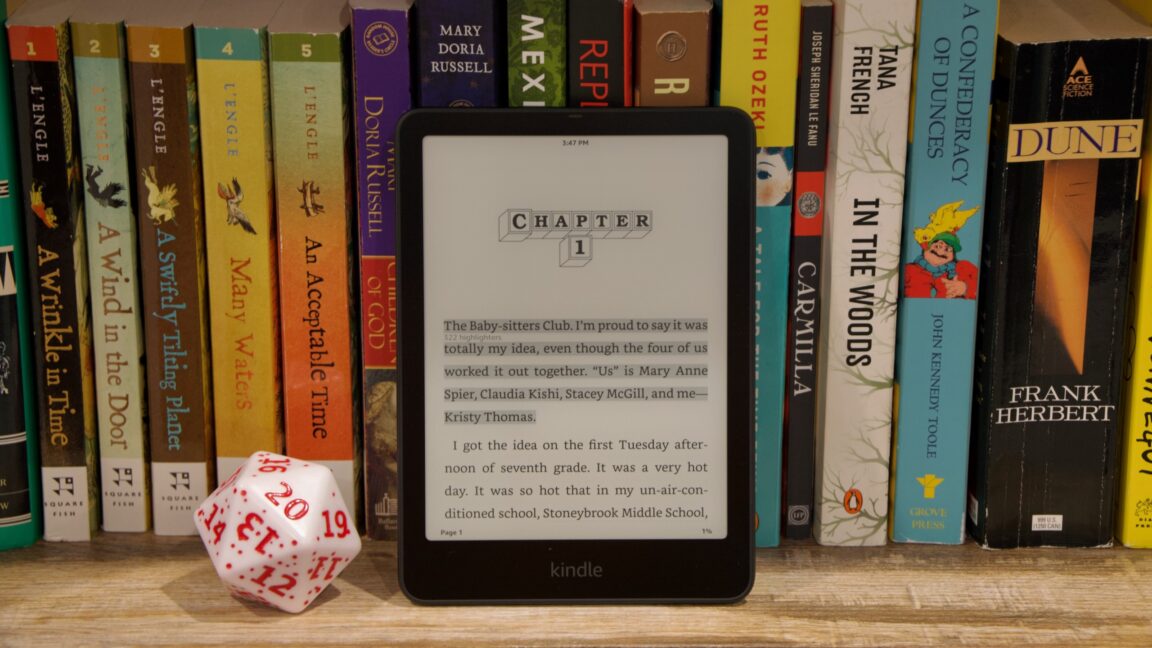 ARSTECHNICA.COMReview: Amazons 2024 Kindle Paperwhite makes the best e-reader a little betterspeed reader Review: Amazons 2024 Kindle Paperwhite makes the best e-reader a little better If you use any Kindle other than the 2021 Paperwhite, this is a huge upgrade. Andrew Cunningham Nov 15, 2024 7:51 am | 205 Credit: Andrew Cunningham Credit: Andrew Cunningham Story textSizeSmallStandardLargeWidth *StandardWideLinksStandardOrange* Subscribers only Learn moreI've never particularly loved Amazon, either as a retail behemoth or as a hardware and software company, but despite that I still probably get more excited about new Kindle releases than I do about most other gadgets at this point.Some of that is because I rely on my Kindle for distraction-free reading and because I'm constantly highlighting things and taking notes, so even minor improvements have a major impact on my day-to-day experience. And some of it is because the Kindle's relatively limited tech has left it without a lot of headroom to shove additional ads or other paid add-ons; they include lockscreen ads and "special offers," but they can be permanently turned off with a nominal $20 fee, and even when you don't turn them off, they don't degrade the device's performance or intrude on the actual reading experience. This isn't to say that Kindles are perfect, just that it's rare that I am roughly the same amount of annoyed by a software platform's ads and tracking than I was a decade ago.Enter the new 12th-generation $160 Kindle Paperwhite, which like most Paperwhites is the Kindle that most people should buy.The 11th-gen Paperwhite update, released in late 2021 for $140, was a big quality-of-life upgrade, with a bigger 6.8-inch screen, adjustable color temperature, USB-C, more frontlight LEDs, and (in the more-expensive Signature Edition) an auto-brightness sensor and wireless charging.The new one has all of that stuff, plus an even bigger 7-inch screen. But the killer feature might be that this is the first Kindle I've used that has ever felt genuinely zippy. Obviously you don't need to run out and buy a new Kindle just because it feels fast. But for owners of older Paperwhitesif you last upgraded, say, back in 2018 when the 10th-gen Paperwhite first went waterproof, or if you have an even older modelin a lot of ways this feels like a totally different e-reader.A fast Kindle? From left to right: 2024 Paperwhite, 2021 Paperwhite, and 2018 Paperwhite. Note not just the increase in screen size, but also how the screen corners get a little more rounded with each release. Credit: Andrew Cunningham I don't want to oversell how fast the new Kindle is, because it's still not like an E-Ink screen can really compete with an LCD or OLED panel for smoothness of animations or UI responsiveness. But even compared to the 2021 Paperwhite, tapping buttons, opening menus, opening books, and turning pages feels considerably snappiernot quite instantaneous, but without the unexplained pauses and hesitation that longtime Kindle owners will be accustomed to. For those who type out notes in their books, even the onscreen keyboard feels fluid and responsive.Compared to the 2018 Paperwhite (again, the first waterproofed model, and the last one with a 6-inch screen and micro USB port), the difference is night and day. While it still feels basically fine for reading books, I find that the older Kindle can sometimes pause for so long when opening menus or switching between things that I wonder if it's still working or whether it's totally locked up and frozen."Kindle benchmarks" aren't really a thing, but I attempted to quantify the performance improvements by running some old browser benchmarks using the Kindle's limited built-in web browser and Google's ancient Octane 2.0 testthe 2018, 2021, and 2024 Kindles are all running the same software update here (5.17.0), so this should be a reasonably good apples-to-apples comparison of single-core processor speed. The new Kindle is actually way faster than older models. Credit: Andrew Cunningham The 2021 Kindle was roughly 30 percent faster than the 2018 Kindle. The new Paperwhite is nearly twice as fast as the 2021 Paperwhite, and well over twice as fast as the 2018 Paperwhite. That alone is enough to explain the tangible difference in responsiveness between the devices.Turning to the new Paperwhite's other improvements: compared side by side, the new screen is appreciably bigger, more noticeably so than the 0.2-inch size difference might suggest. And it doesn't make the Paperwhite much larger, though it is a tiny bit taller in a way that will wreck compatibility with existing cases. But you only really appreciate the upgrade if you're coming from one of the older 6-inch Kindles.Amazon's product pages and press releases brag of improved contrast, and the new Paperwhite does produce slightly deeper, less-washed-out shades of black than the 2021 model. Most of the time, you'll only really notice this if you're using the two devices side by side. But if you use Dark Mode frequently, the upgrade is more noticeable, since the background can get quite a bit darker while keeping the text brighter and easier to read. The new Paperwhite, like the 2021 model, uses USB-C for charging. Wireless charging is an optional feature of the more expensive Signature Edition. Credit: Andrew Cunningham To my eyes, the screen brightness and the warm light in the new Kindle look identical to the one from 2021and after years of using a Kindle with a warm light regularly, I would hate to have to go back to a model without one. The bluish default color temperature makes it look less like paper, and it's a bit harder on the eyes in dim lighting.The new Paperwhite still has a USB-C port, like the 2021 Paperwhite, and still has a soft-touch texture on the back that's pleasant to hold for long reading sessions.The upgraders Kindle The back of the new Kindle Paperwhite. Credit: Andrew Cunningham If you're using pretty much any Kindle other than the 2021 Kindle Paperwhite, this new version is going to feel like a huge improvement over whatever you're currently using (unless you're a physical button holdout, but for better or worse that decision has clearly been made). The 7-inch screen is a lot bigger than whatever you're using, the warm light is easier on the eyes, the optional auto-brightness sensor and wireless charging capability are nice-to-haves if you want to pay more for the Signature Edition. And all of that frustrating Kindle slowdown is just gone, thanks to a considerably faster processor.If you're using the 2021 Kindle Paperwhite, on the other hand, you probably don't need to consider an upgrade. There are things I really like about the new Paperwhite, but it's really just building on the foundation laid by the 2021 model. In fact, the availability of a newer model might make a used or refurbished 2021 Paperwhite the best entry-level Kindle you can buynot the marginally improved but still much less capable $110 baseline Kindle that Amazon just introduced.In any case, the new Paperwhite is still the best combination of features and price that Amazon offers in its e-reader lineup, despite the small price increase. The cheaper Kindle is smaller, not waterproof, and has no warm light; we're reserving judgment on the Kindle Colorsoft until we can try it for ourselves, but early user reviews complain about the crispness of black-and-white text and other things that may or may not be software bugs. If you just want to read a book, the Paperwhite is still the best way to do it.The goodA great reading experience backed up by Kindle's strong library and app ecosystem.Larger screen.Ads are relatively easy to ignore and inexpensive to permanently dismiss.Improved display contrast isn't super noticeable most of the time, but it does make a difference in dark mode.The badNo interesting screen tech upgrades like color or pen supportthis one's just for reading.Breaks compatibility with older Kindle accessories.The uglyThe price keeps creeping upward with every refresh.Andrew CunninghamSenior Technology ReporterAndrew CunninghamSenior Technology Reporter Andrew is a Senior Technology Reporter at Ars Technica, with a focus on consumer tech including computer hardware and in-depth reviews of operating systems like Windows and macOS. Andrew lives in Philadelphia and co-hosts a weekly book podcast called Overdue. 205 Comments0 Σχόλια 0 Μοιράστηκε 207 Views
ARSTECHNICA.COMReview: Amazons 2024 Kindle Paperwhite makes the best e-reader a little betterspeed reader Review: Amazons 2024 Kindle Paperwhite makes the best e-reader a little better If you use any Kindle other than the 2021 Paperwhite, this is a huge upgrade. Andrew Cunningham Nov 15, 2024 7:51 am | 205 Credit: Andrew Cunningham Credit: Andrew Cunningham Story textSizeSmallStandardLargeWidth *StandardWideLinksStandardOrange* Subscribers only Learn moreI've never particularly loved Amazon, either as a retail behemoth or as a hardware and software company, but despite that I still probably get more excited about new Kindle releases than I do about most other gadgets at this point.Some of that is because I rely on my Kindle for distraction-free reading and because I'm constantly highlighting things and taking notes, so even minor improvements have a major impact on my day-to-day experience. And some of it is because the Kindle's relatively limited tech has left it without a lot of headroom to shove additional ads or other paid add-ons; they include lockscreen ads and "special offers," but they can be permanently turned off with a nominal $20 fee, and even when you don't turn them off, they don't degrade the device's performance or intrude on the actual reading experience. This isn't to say that Kindles are perfect, just that it's rare that I am roughly the same amount of annoyed by a software platform's ads and tracking than I was a decade ago.Enter the new 12th-generation $160 Kindle Paperwhite, which like most Paperwhites is the Kindle that most people should buy.The 11th-gen Paperwhite update, released in late 2021 for $140, was a big quality-of-life upgrade, with a bigger 6.8-inch screen, adjustable color temperature, USB-C, more frontlight LEDs, and (in the more-expensive Signature Edition) an auto-brightness sensor and wireless charging.The new one has all of that stuff, plus an even bigger 7-inch screen. But the killer feature might be that this is the first Kindle I've used that has ever felt genuinely zippy. Obviously you don't need to run out and buy a new Kindle just because it feels fast. But for owners of older Paperwhitesif you last upgraded, say, back in 2018 when the 10th-gen Paperwhite first went waterproof, or if you have an even older modelin a lot of ways this feels like a totally different e-reader.A fast Kindle? From left to right: 2024 Paperwhite, 2021 Paperwhite, and 2018 Paperwhite. Note not just the increase in screen size, but also how the screen corners get a little more rounded with each release. Credit: Andrew Cunningham I don't want to oversell how fast the new Kindle is, because it's still not like an E-Ink screen can really compete with an LCD or OLED panel for smoothness of animations or UI responsiveness. But even compared to the 2021 Paperwhite, tapping buttons, opening menus, opening books, and turning pages feels considerably snappiernot quite instantaneous, but without the unexplained pauses and hesitation that longtime Kindle owners will be accustomed to. For those who type out notes in their books, even the onscreen keyboard feels fluid and responsive.Compared to the 2018 Paperwhite (again, the first waterproofed model, and the last one with a 6-inch screen and micro USB port), the difference is night and day. While it still feels basically fine for reading books, I find that the older Kindle can sometimes pause for so long when opening menus or switching between things that I wonder if it's still working or whether it's totally locked up and frozen."Kindle benchmarks" aren't really a thing, but I attempted to quantify the performance improvements by running some old browser benchmarks using the Kindle's limited built-in web browser and Google's ancient Octane 2.0 testthe 2018, 2021, and 2024 Kindles are all running the same software update here (5.17.0), so this should be a reasonably good apples-to-apples comparison of single-core processor speed. The new Kindle is actually way faster than older models. Credit: Andrew Cunningham The 2021 Kindle was roughly 30 percent faster than the 2018 Kindle. The new Paperwhite is nearly twice as fast as the 2021 Paperwhite, and well over twice as fast as the 2018 Paperwhite. That alone is enough to explain the tangible difference in responsiveness between the devices.Turning to the new Paperwhite's other improvements: compared side by side, the new screen is appreciably bigger, more noticeably so than the 0.2-inch size difference might suggest. And it doesn't make the Paperwhite much larger, though it is a tiny bit taller in a way that will wreck compatibility with existing cases. But you only really appreciate the upgrade if you're coming from one of the older 6-inch Kindles.Amazon's product pages and press releases brag of improved contrast, and the new Paperwhite does produce slightly deeper, less-washed-out shades of black than the 2021 model. Most of the time, you'll only really notice this if you're using the two devices side by side. But if you use Dark Mode frequently, the upgrade is more noticeable, since the background can get quite a bit darker while keeping the text brighter and easier to read. The new Paperwhite, like the 2021 model, uses USB-C for charging. Wireless charging is an optional feature of the more expensive Signature Edition. Credit: Andrew Cunningham To my eyes, the screen brightness and the warm light in the new Kindle look identical to the one from 2021and after years of using a Kindle with a warm light regularly, I would hate to have to go back to a model without one. The bluish default color temperature makes it look less like paper, and it's a bit harder on the eyes in dim lighting.The new Paperwhite still has a USB-C port, like the 2021 Paperwhite, and still has a soft-touch texture on the back that's pleasant to hold for long reading sessions.The upgraders Kindle The back of the new Kindle Paperwhite. Credit: Andrew Cunningham If you're using pretty much any Kindle other than the 2021 Kindle Paperwhite, this new version is going to feel like a huge improvement over whatever you're currently using (unless you're a physical button holdout, but for better or worse that decision has clearly been made). The 7-inch screen is a lot bigger than whatever you're using, the warm light is easier on the eyes, the optional auto-brightness sensor and wireless charging capability are nice-to-haves if you want to pay more for the Signature Edition. And all of that frustrating Kindle slowdown is just gone, thanks to a considerably faster processor.If you're using the 2021 Kindle Paperwhite, on the other hand, you probably don't need to consider an upgrade. There are things I really like about the new Paperwhite, but it's really just building on the foundation laid by the 2021 model. In fact, the availability of a newer model might make a used or refurbished 2021 Paperwhite the best entry-level Kindle you can buynot the marginally improved but still much less capable $110 baseline Kindle that Amazon just introduced.In any case, the new Paperwhite is still the best combination of features and price that Amazon offers in its e-reader lineup, despite the small price increase. The cheaper Kindle is smaller, not waterproof, and has no warm light; we're reserving judgment on the Kindle Colorsoft until we can try it for ourselves, but early user reviews complain about the crispness of black-and-white text and other things that may or may not be software bugs. If you just want to read a book, the Paperwhite is still the best way to do it.The goodA great reading experience backed up by Kindle's strong library and app ecosystem.Larger screen.Ads are relatively easy to ignore and inexpensive to permanently dismiss.Improved display contrast isn't super noticeable most of the time, but it does make a difference in dark mode.The badNo interesting screen tech upgrades like color or pen supportthis one's just for reading.Breaks compatibility with older Kindle accessories.The uglyThe price keeps creeping upward with every refresh.Andrew CunninghamSenior Technology ReporterAndrew CunninghamSenior Technology Reporter Andrew is a Senior Technology Reporter at Ars Technica, with a focus on consumer tech including computer hardware and in-depth reviews of operating systems like Windows and macOS. Andrew lives in Philadelphia and co-hosts a weekly book podcast called Overdue. 205 Comments0 Σχόλια 0 Μοιράστηκε 207 Views -
 WWW.TECHNOLOGYREVIEW.COMGoogle DeepMind has a new way to look inside an AIs mindAI has led to breakthroughs in drug discovery and robotics and is in the process of entirely revolutionizing how we interact with machines and the web. The only problem is we dont know exactly how it works, or why it works so well. We have a fair idea, but the details are too complex to unpick. Thats a problem: It could lead us to deploy an AI system in a highly sensitive field like medicine without understanding that it could have critical flaws embedded in its workings. A team at Google DeepMind that studies something called mechanistic interpretability has been working on new ways to let us peer under the hood. At the end of July, it released Gemma Scope, a tool to help researchers understand what is happening when AI is generating an output. The hope is that if we have a better understanding of what is happening inside an AI model, well be able to control its outputs more effectively, leading to better AI systems in the future. I want to be able to look inside a model and see if its being deceptive, says Neel Nanda, who runs the mechanistic interpretability team at Google DeepMind. It seems like being able to read a models mind should help. Mechanistic interpretability, also known as mech interp, is a new research field that aims to understand how neural networks actually work. At the moment, very basically, we put inputs into a model in the form of a lot of data, and then we get a bunch of model weights at the end of training. These are the parameters that determine how a model makes decisions. We have some idea of whats happening between the inputs and the model weights: Essentially, the AI is finding patterns in the data and making conclusions from those patterns, but these patterns can be incredibly complex and often very hard for humans to interpret. Its like a teacher reviewing the answers to a complex math problem on a test. The studentthe AI, in this casewrote down the correct answer, but the work looks like a bunch of squiggly lines. This example assumes the AI is always getting the correct answer, but thats not always true; the AI student may have found an irrelevant pattern that its assuming is valid. For example, some current AI systems will give you the result that 9.11 is bigger than 9.8. Different methods developed in the field of mechanistic interpretability are beginning to shed a little bit of light on what may be happening, essentially making sense of the squiggly lines. A key goal of mechanistic interpretability is trying to reverse-engineer the algorithms inside these systems, says Nanda. We give the model a prompt, like Write a poem, and then it writes some rhyming lines. What is the algorithm by which it did this? Wed love to understand it. To find featuresor categories of data that represent a larger conceptin its AI model, Gemma, DeepMind ran a tool known as a sparse autoencoder on each of its layers. You can think of a sparse autoencoder as a microscope that zooms in on those layers and lets you look at their details. For example, if you prompt Gemma about a chihuahua, it will trigger the dogs feature, lighting up what the model knows about dogs. The reason it is considered sparse is that its limiting the number of neurons used, basically pushing for a more efficient and generalized representation of the data. The tricky part of sparse autoencoders is deciding how granular you want to get. Think again about the microscope. You can magnify something to an extreme degree, but it may make what youre looking at impossible for a human to interpret. But if you zoom too far out, you may be limiting what interesting things you can see and discover. DeepMinds solution was to run sparse autoencoders of different sizes, varying the number of features they want the autoencoder to find. The goal was not for DeepMinds researchers to thoroughly analyze the results on their own. Gemma and the autoencoders are open-source, so this project was aimed more at spurring interested researchers to look at what the sparse autoencoders found and hopefully make new insights into the model's internal logic. Since DeepMind ran autoencoders on each layer of their model, a researcher could map the progression from input to output to a degree we havent seen before. This is really exciting for interpretability researchers, says Josh Batson, a researcher at Anthropic. If you have this model that youve open-sourced for people to study, it means that a bunch of interpretability research can now be done on the back of those sparse autoencoders. It lowers the barrier to entry to people learning from these methods. Neuronpedia, a platform for mechanistic interpretability, partnered with DeepMind in July to build a demo of Gemma Scope that you can play around with right now. In the demo, you can test out different prompts and see how the model breaks up your prompt and what activations your prompt lights up. You can also mess around with the model. For example, if you turn the feature about dogs way up and then ask the model a question about US presidents, Gemma will find some way to weave in random babble about dogs, or the model may just start barking at you. One interesting thing about sparse autoencoders is that they are unsupervised, meaning they find features on their own. That leads to surprising discoveries about how the models break down human concepts. My personal favorite feature is the cringe feature, says Joseph Bloom, science lead at Neuronpedia. It seems to appear in negative criticism of text and movies. Its just a great example of tracking things that are so human on some level. You can search for concepts on Neuronpedia and it will highlight what features are being activated on specific tokens, or words, and how strongly each one is activated. If you read the text and you see whats highlighted in green, thats when the model thinks the cringe concept is most relevant. The most active example for cringe is somebody preaching at someone else, says Bloom. Some features are proving easier to track than others. One of the most important features that you would want to find for a model is deception, says Johnny Lin, founder of Neuronpedia. Its not super easy to find: Oh, theres the feature that fires when its lying to us. From what Ive seen, it hasnt been the case that we can find deception and ban it. DeepMinds research is similar to what another AI company, Anthropic, did back in May with Golden Gate Claude. It used sparse autoencoders to find the parts of Claude, their model, that lit up when discussing the Golden Gate Bridge in San Francisco. It then amplified the activations related to the bridge to the point where Claude literally identified not as Claude, an AI model, but as the physical Golden Gate Bridge and would respond to prompts as the bridge. Although it may just seem quirky, mechanistic interpretability research may prove incredibly useful. As a tool for understanding how the model generalizes and what level of abstraction its working at, these features are really helpful, says Batson. For example, a team lead by Samuel Marks, now at Anthropic, used sparse autoencoders to find features that showed a particular model was associating certain professions with a specific gender. They then turned off these gender features to reduce bias in the model. This experiment was done on a very small model, so its unclear if the work will apply to a much larger model. Mechanistic interpretability research can also give us insights into why AI makes errors. In the case of the assertion that 9.11 is larger than 9.8, researchers from Transluce saw that the question was triggering the parts of an AI model related to Bible verses and September 11. The researchers concluded the AI could be interpreting the numbers as dates, asserting the later date, 9/11, as greater than 9/8. And in a lot of books like religious texts, section 9.11 comes after section 9.8, which may be why the AI thinks of it as greater. Once they knew why the AI made this error, the researchers tuned down the AI's activations on Bible verses and September 11, which led to the model giving the correct answer when prompted again on whether 9.11 is larger than 9.8. There are also other potential applications. Currently, a system-level prompt is built into LLMs to deal with situations like users who ask how to build a bomb. When you ask ChatGPT a question, the model is first secretly prompted by OpenAI to refrain from telling you how to make bombs or do other nefarious things. But its easy for users to jailbreak AI models with clever prompts, bypassing any restrictions. If the creators of the models are able to see where in an AI the bomb-building knowledge is, they can theoretically turn off those nodes permanently. Then even the most cleverly written prompt wouldnt elicit an answer about how to build a bomb, because the AI would literally have no information about how to build a bomb in its system. This type of granularity and precise control are easy to imagine but extremely hard to achieve with the current state of mechanistic interpretability. A limitation is the steering [influencing a model by adjusting its parameters] is just not working that well, and so when you steer to reduce violence in a model, it ends up completely lobotomizing its knowledge in martial arts. Theres a lot of refinement to be done in steering, says Lin. The knowledge of bomb making, for example, isnt just a simple on-and-off switch in an AI model. It most likely is woven into multiple parts of the model, and turning it off would probably involve hampering the AIs knowledge of chemistry. Any tinkering may have benefits but also significant trade-offs. That said, if we are able to dig deeper and peer more clearly into the mind of AI, DeepMind and others are hopeful that mechanistic interpretability could represent a plausible path to alignmentthe process of making sure AI is actually doing what we want it to do.0 Σχόλια 0 Μοιράστηκε 191 Views
WWW.TECHNOLOGYREVIEW.COMGoogle DeepMind has a new way to look inside an AIs mindAI has led to breakthroughs in drug discovery and robotics and is in the process of entirely revolutionizing how we interact with machines and the web. The only problem is we dont know exactly how it works, or why it works so well. We have a fair idea, but the details are too complex to unpick. Thats a problem: It could lead us to deploy an AI system in a highly sensitive field like medicine without understanding that it could have critical flaws embedded in its workings. A team at Google DeepMind that studies something called mechanistic interpretability has been working on new ways to let us peer under the hood. At the end of July, it released Gemma Scope, a tool to help researchers understand what is happening when AI is generating an output. The hope is that if we have a better understanding of what is happening inside an AI model, well be able to control its outputs more effectively, leading to better AI systems in the future. I want to be able to look inside a model and see if its being deceptive, says Neel Nanda, who runs the mechanistic interpretability team at Google DeepMind. It seems like being able to read a models mind should help. Mechanistic interpretability, also known as mech interp, is a new research field that aims to understand how neural networks actually work. At the moment, very basically, we put inputs into a model in the form of a lot of data, and then we get a bunch of model weights at the end of training. These are the parameters that determine how a model makes decisions. We have some idea of whats happening between the inputs and the model weights: Essentially, the AI is finding patterns in the data and making conclusions from those patterns, but these patterns can be incredibly complex and often very hard for humans to interpret. Its like a teacher reviewing the answers to a complex math problem on a test. The studentthe AI, in this casewrote down the correct answer, but the work looks like a bunch of squiggly lines. This example assumes the AI is always getting the correct answer, but thats not always true; the AI student may have found an irrelevant pattern that its assuming is valid. For example, some current AI systems will give you the result that 9.11 is bigger than 9.8. Different methods developed in the field of mechanistic interpretability are beginning to shed a little bit of light on what may be happening, essentially making sense of the squiggly lines. A key goal of mechanistic interpretability is trying to reverse-engineer the algorithms inside these systems, says Nanda. We give the model a prompt, like Write a poem, and then it writes some rhyming lines. What is the algorithm by which it did this? Wed love to understand it. To find featuresor categories of data that represent a larger conceptin its AI model, Gemma, DeepMind ran a tool known as a sparse autoencoder on each of its layers. You can think of a sparse autoencoder as a microscope that zooms in on those layers and lets you look at their details. For example, if you prompt Gemma about a chihuahua, it will trigger the dogs feature, lighting up what the model knows about dogs. The reason it is considered sparse is that its limiting the number of neurons used, basically pushing for a more efficient and generalized representation of the data. The tricky part of sparse autoencoders is deciding how granular you want to get. Think again about the microscope. You can magnify something to an extreme degree, but it may make what youre looking at impossible for a human to interpret. But if you zoom too far out, you may be limiting what interesting things you can see and discover. DeepMinds solution was to run sparse autoencoders of different sizes, varying the number of features they want the autoencoder to find. The goal was not for DeepMinds researchers to thoroughly analyze the results on their own. Gemma and the autoencoders are open-source, so this project was aimed more at spurring interested researchers to look at what the sparse autoencoders found and hopefully make new insights into the model's internal logic. Since DeepMind ran autoencoders on each layer of their model, a researcher could map the progression from input to output to a degree we havent seen before. This is really exciting for interpretability researchers, says Josh Batson, a researcher at Anthropic. If you have this model that youve open-sourced for people to study, it means that a bunch of interpretability research can now be done on the back of those sparse autoencoders. It lowers the barrier to entry to people learning from these methods. Neuronpedia, a platform for mechanistic interpretability, partnered with DeepMind in July to build a demo of Gemma Scope that you can play around with right now. In the demo, you can test out different prompts and see how the model breaks up your prompt and what activations your prompt lights up. You can also mess around with the model. For example, if you turn the feature about dogs way up and then ask the model a question about US presidents, Gemma will find some way to weave in random babble about dogs, or the model may just start barking at you. One interesting thing about sparse autoencoders is that they are unsupervised, meaning they find features on their own. That leads to surprising discoveries about how the models break down human concepts. My personal favorite feature is the cringe feature, says Joseph Bloom, science lead at Neuronpedia. It seems to appear in negative criticism of text and movies. Its just a great example of tracking things that are so human on some level. You can search for concepts on Neuronpedia and it will highlight what features are being activated on specific tokens, or words, and how strongly each one is activated. If you read the text and you see whats highlighted in green, thats when the model thinks the cringe concept is most relevant. The most active example for cringe is somebody preaching at someone else, says Bloom. Some features are proving easier to track than others. One of the most important features that you would want to find for a model is deception, says Johnny Lin, founder of Neuronpedia. Its not super easy to find: Oh, theres the feature that fires when its lying to us. From what Ive seen, it hasnt been the case that we can find deception and ban it. DeepMinds research is similar to what another AI company, Anthropic, did back in May with Golden Gate Claude. It used sparse autoencoders to find the parts of Claude, their model, that lit up when discussing the Golden Gate Bridge in San Francisco. It then amplified the activations related to the bridge to the point where Claude literally identified not as Claude, an AI model, but as the physical Golden Gate Bridge and would respond to prompts as the bridge. Although it may just seem quirky, mechanistic interpretability research may prove incredibly useful. As a tool for understanding how the model generalizes and what level of abstraction its working at, these features are really helpful, says Batson. For example, a team lead by Samuel Marks, now at Anthropic, used sparse autoencoders to find features that showed a particular model was associating certain professions with a specific gender. They then turned off these gender features to reduce bias in the model. This experiment was done on a very small model, so its unclear if the work will apply to a much larger model. Mechanistic interpretability research can also give us insights into why AI makes errors. In the case of the assertion that 9.11 is larger than 9.8, researchers from Transluce saw that the question was triggering the parts of an AI model related to Bible verses and September 11. The researchers concluded the AI could be interpreting the numbers as dates, asserting the later date, 9/11, as greater than 9/8. And in a lot of books like religious texts, section 9.11 comes after section 9.8, which may be why the AI thinks of it as greater. Once they knew why the AI made this error, the researchers tuned down the AI's activations on Bible verses and September 11, which led to the model giving the correct answer when prompted again on whether 9.11 is larger than 9.8. There are also other potential applications. Currently, a system-level prompt is built into LLMs to deal with situations like users who ask how to build a bomb. When you ask ChatGPT a question, the model is first secretly prompted by OpenAI to refrain from telling you how to make bombs or do other nefarious things. But its easy for users to jailbreak AI models with clever prompts, bypassing any restrictions. If the creators of the models are able to see where in an AI the bomb-building knowledge is, they can theoretically turn off those nodes permanently. Then even the most cleverly written prompt wouldnt elicit an answer about how to build a bomb, because the AI would literally have no information about how to build a bomb in its system. This type of granularity and precise control are easy to imagine but extremely hard to achieve with the current state of mechanistic interpretability. A limitation is the steering [influencing a model by adjusting its parameters] is just not working that well, and so when you steer to reduce violence in a model, it ends up completely lobotomizing its knowledge in martial arts. Theres a lot of refinement to be done in steering, says Lin. The knowledge of bomb making, for example, isnt just a simple on-and-off switch in an AI model. It most likely is woven into multiple parts of the model, and turning it off would probably involve hampering the AIs knowledge of chemistry. Any tinkering may have benefits but also significant trade-offs. That said, if we are able to dig deeper and peer more clearly into the mind of AI, DeepMind and others are hopeful that mechanistic interpretability could represent a plausible path to alignmentthe process of making sure AI is actually doing what we want it to do.0 Σχόλια 0 Μοιράστηκε 191 Views -
WWW.BUSINESSINSIDER.COMA product manager shares the rsum that got him a $300,000 job at Amazon — and 3 regrets about it, including writing that sounds 'very pompous'Siddharth Kashiramka joined Amazon in 2022 as a product manager for AI projects.Looking back, he thought his rsum highlighted his impact but he would not write in the third-person now.And he would stick to one page, the standard recommended rsum length.Siddharth Kashiramka was six years into his post-Masters career when he began considering his next move.He worked as a product manager at Capital One and was previously a consultant at PwC. Some of his colleagues had gone to Amazon, but he didn't want to uproot his life from Virginia to Seattle. Then he was approached to work with artificial intelligence at Amazon no move required.To prepare for his interview, Kashiramka networked with contacts who had made a similar transition and spent a month practicing for interviews, doing mock sessions on a career service platform.After several rounds of interviews, Kashiramka landed a product management role at Amazon in 2022. The role came with about $300,000 in annual compensation, a mix of base salary and stock options.As a hiring manager, Kashiramka said that while rsums are a small part of the overall hiring process, they can still be an important decision-making tool."I remember an instance where there were two equally good candidates for a position. Both of them cleared the final round of interviews, but the offer had to be given to only one," Kashiramka said. "Ultimately, the decision hinged on the candidate with the most polished rsum."Here is the rsum he used to apply to Amazon and other Big Tech companies. It wasn't perfect he told Business Insider he would change three major components.Looking back on the rsum, he said three things work well:1. Talk about impact: He gives a high-level description of past roles, followed by his work and its impact.2. Summarize: "The summary is very unique to me," he said. "You can't copy-paste it to someone else." In the future, he would also add a short section talking about his external mentorship efforts and academic journal contributions, which he has been doing more actively since 2022.3. Show variety: Throughout the rsum, Kashiramka used a range of keywords, including "leveraged," "delivered," "established," and "collaborated." "Unintentionally this also optimizes for the ATS systems as well," he said about the application tracking systems that digitally parse rsums for keywords.What he would changeWhile the rsum got him interviews at Meta, Amazon, and Google, there are still a few things he would change moving forward:1. One page rsum: "I think the rsum should be one page," he said about keeping the document short. "That was a big red flag for me here in this rsum." Kashiramka added that his rsums for PwC and Capital One, where he worked before Amazon, were both one page, and he would return to that length in the future.2. Use first-person voice: Kashiramka said another mistake was writing about himself in the third person because it sounds less personal. "It seems very pompous, to be honest," he said. "I'm like: 'Who am I talking about here?'"3. Attention to detail: "I have made a few grammatical mistakes in this," he said. He recommends using a proofreading tool and getting another set of human eyes on the document.Kashiramka said that while there were grammatical errors, he was careful to be consistent in formatting, such as not using periods anywhere.Kashiramka is a senior product manager at Amazon's office in Crystal City,Virginia. Business Insider has verified his employment history and compensation.0 Σχόλια 0 Μοιράστηκε 195 Views
-
WWW.BUSINESSINSIDER.COMI raised my kids across 5 countries before they turned 10. Now, we're going through reverse culture shock in Minnesota.Kate Stockinger grew up in the UK and met her now-husband in New York.The couple raised their two daughters in five cities across four continents before deciding to settle in Minnesota.She finds people in her husband's home state welcoming but her kids had trouble settling in.Two truths and a lie. My daughter Freya was 10, it was the first day at her new school in Minnesota, and it was her turn to share: "I've lived in 5 countries and 4 continents; I like cheese; I lived in India when I was 2 years old," she said.The classmates debated between whether the lie was the number of countries or that she'd lived in India until she shouted out that it was the cheese she'd never been a fan.In Minnesota, new kids rarely show up, and when they do, they're usually coming from nearby. My family moved to Minnesota in July, and it's taking time for my two daughters and me to settle down.I grew up in the UK. I met my now-husband Andy during acollege internshipat a private golf club in New York. He had recently moved to the Big Apple from Minnesota.We fell in love, got married, and he soon started getting job placements working at different golf courses around the world. Over the next 10 years, we had two daughters, moved five times, and lived in five cities across four continents. After our time in Egypt, and with our eldest daughter not getting what she needed from her international school, we decided to hang up our expat life and move "home" to Minnesota.We decided that this was where our kids needed to live to get the education we wanted for them. Taking this leap has been our scariest decision. My husband quit his job, and we moved to the US with nothing lined up. We were lucky to have the support of family and friends both in the US and back in the UK.Of course, with all of this change, there have been some high highs and some low lows. The last picture Stockinger's family took in Egypt before moving. Kate Stockinger Culture shock started at TargetStores in the US really do have everything but sometimes there's too much to choose from.Target is somewhere I have to be in the right mood to go, as the variety of chips, yogurt, and out-of-season fruit they have is mind-blowing. In countries we have lived in before, it's always been seasonal and a treat to have berries that were not frozen. Recent trips to Target with my kids can take at least an hour, as my daughters want to peruse every inch of the store,I appreciate that I no longer have to pay crazy amounts of money for skincare or shampoo, but now my daughter has discovered a whole aisle dedicated to kids' skincare and makeup.Kids struggling to fit inThe statement "Minnesota Nice" holds up. Everyone here is so friendly and willing to help. It's a stark and welcome contrast compared to some of the communities where we previously lived.Despite this, my kids have had trouble settling in. Freya has found it hard to fit in with kids at school, as the majority of children in her class have been together since Pre-K.Hearing her tell me that she played on her own during recess has been heartbreaking. When we lived abroad, it was easier, as there were always new kids, and the schools tended to deal with it a little better.Winter is comingIn the past, our vacation visits to Minnesota typically took place in the summer. I have never experienced a proper Minnesotan Winter.In Anna and Elsa's words, my daughters and I are absolutely buzzing to be able to say, "Do you wanna build a snowman?" But my husband, his family, and our friends are waiting for our attitudes to turn when those daylight hours become less, and the damp, wet reality of that snow hits. As I am forever the optimist, I hope to see the positive even when we have to face the dull, dark days.We are proud that our kids started their lives as global citizens and hope to continue their experience by enjoying family vacations once we have our feet firmly on the ground. This is the fastest we have settled into somewhere, proving to ourselves that we are done with expat life and ready to have neighbors in a cul-de-sac.0 Σχόλια 0 Μοιράστηκε 196 Views
-
 GIZMODO.COMLooking as Good as New, This MacBook Air Is Cheaper Than a Pair of AirPods ProIn the world of laptops, Apples MacBook Air has long been celebrated for its sleek design and impressive performance. If youve been eyeing a MacBook but are hesitant to splurge on a brand-new model, StackSocial has an incredible early Black Friday deal that you wont want to miss: For just $249, you can grab a refurbished 2017 MacBook Air with 128 GB of storage, a price thats a staggering reduction from its original retail price of $999. While its true that you wont find this model at its original price anymore, the value it offers at this discount is undeniable.See at StackSocialThis Grade A refurbished MacBook Air is in near-mint condition and showcases minimal signs of wear and tear: Its as close to new as you can get without paying the premium price tag. For anyone who wants the Apple experience without paying the full price, this laptop is an excellent choice. The 2017 model features a reliable Intel Core i5 processor running at 1.8 GHz and it can handle everyday tasks with ease. Whether youre browsing the web, streaming videos or working on documents, this machine delivers smooth performance.Affordable Yet Powerful LaptopThis MacBook Air on sale at StackSocial comes equipped with 128 GB of solid-state storage which provides ample space for your files and applications. If you find yourself needing more storage down the line, you can easily expand it by connecting an external drive via one of its USB-A ports. The Intel HD Graphics 6000 card enhances your visual experience and makes it perfect for light gaming and media consumption on its 13.3-inch screen.Whats great is that this MacBook Air can last up to 12 hours on a single charge and allows you to work or play throughout the day without constantly searching for an outlet. This makes it an ideal companion for students or professionals who are always on the go. Portability is another strong suit of the MacBook Air: It weights just 2.96 pounds and has a slim profile (only 0.11 inches thick when closed) si its easy to slip into a backpack or briefcase.While there are many budget laptops available in the market today, most fall short in terms of quality and reliability compared to the MacBook Air. Many cheaper options are often heavy and lack durability and lead users back to the search for another laptop sooner than theyd like. Choosing this Grade-A MacBook Air from StackSocial means investing in a product known for its longevity and performance at a price point that rivals lower-end PCs.Moreover, purchasing refurbished electronics is not only budget-friendly but also environmentally conscious. By opting for a refurbished device, you contribute to reducing electronic waste while still enjoying high-quality technology. This particular MacBook Air comes with a 90-day warranty covering parts and labor which gives you peace of mind with your purchase.See at StackSocial0 Σχόλια 0 Μοιράστηκε 156 Views
GIZMODO.COMLooking as Good as New, This MacBook Air Is Cheaper Than a Pair of AirPods ProIn the world of laptops, Apples MacBook Air has long been celebrated for its sleek design and impressive performance. If youve been eyeing a MacBook but are hesitant to splurge on a brand-new model, StackSocial has an incredible early Black Friday deal that you wont want to miss: For just $249, you can grab a refurbished 2017 MacBook Air with 128 GB of storage, a price thats a staggering reduction from its original retail price of $999. While its true that you wont find this model at its original price anymore, the value it offers at this discount is undeniable.See at StackSocialThis Grade A refurbished MacBook Air is in near-mint condition and showcases minimal signs of wear and tear: Its as close to new as you can get without paying the premium price tag. For anyone who wants the Apple experience without paying the full price, this laptop is an excellent choice. The 2017 model features a reliable Intel Core i5 processor running at 1.8 GHz and it can handle everyday tasks with ease. Whether youre browsing the web, streaming videos or working on documents, this machine delivers smooth performance.Affordable Yet Powerful LaptopThis MacBook Air on sale at StackSocial comes equipped with 128 GB of solid-state storage which provides ample space for your files and applications. If you find yourself needing more storage down the line, you can easily expand it by connecting an external drive via one of its USB-A ports. The Intel HD Graphics 6000 card enhances your visual experience and makes it perfect for light gaming and media consumption on its 13.3-inch screen.Whats great is that this MacBook Air can last up to 12 hours on a single charge and allows you to work or play throughout the day without constantly searching for an outlet. This makes it an ideal companion for students or professionals who are always on the go. Portability is another strong suit of the MacBook Air: It weights just 2.96 pounds and has a slim profile (only 0.11 inches thick when closed) si its easy to slip into a backpack or briefcase.While there are many budget laptops available in the market today, most fall short in terms of quality and reliability compared to the MacBook Air. Many cheaper options are often heavy and lack durability and lead users back to the search for another laptop sooner than theyd like. Choosing this Grade-A MacBook Air from StackSocial means investing in a product known for its longevity and performance at a price point that rivals lower-end PCs.Moreover, purchasing refurbished electronics is not only budget-friendly but also environmentally conscious. By opting for a refurbished device, you contribute to reducing electronic waste while still enjoying high-quality technology. This particular MacBook Air comes with a 90-day warranty covering parts and labor which gives you peace of mind with your purchase.See at StackSocial0 Σχόλια 0 Μοιράστηκε 156 Views -
 GIZMODO.COMAmazons Fine With Red One Not Being a Box Office HitIts time for the holiday movie season, and Amazons kicking things off with its action-comedy feature Red One. The film has a lot of star power behind it, with Dwayne Johnson and Chris Evans playing an odd couple tasked with saving a kidnapped Santa Claus (J.K. Simmons), and its trailers have made it seem like it could be either surprisingly good or a complete mess. And the answer appears to be kind of both? Reaction-wise, audiences have taken toRed Onemuch more than critics, most of whom did not really care for it. Thats further reflected in its just okay box office: of the films $84.1 million box office, $34.1 million of that was domestic, and generally in line with its projected $30-35 million range. However, as noted by Variety, the movie itself reportedly cost a hefty $250 million to make, and its biggest accomplishment is halting Venom: The Last Dances continued domestic reign over the last few weeks. Time might not also be on Red Ones side, since its about to be a pretty crowded time at the movies between Wicked: Part I, Gladiator II,and Moana 2 So depending on your thinking, it might be curtains for Red Onestheatrical run in the near futurethough Amazon MGMs theatrical head isnt quite looking to throw in the towel just yet. Amidst those other movies, he believes the Christmas flick offers something a little different than those movies, but stopped short of saying what that something differentis. But even if the movies not a box office hit, the studios more confident itll land with audiences once it hits Prime Video, similar to how Aprils Road Houseremake was such a streaming hit to get a sequel greenlit. According to him, Amazon films getting theatrical runs can help cover the marketing costs ahead of streaming, which is reason enough to let them play on the big screen for a few weeks.WheneverRed Onehits Prime Video, the real way to determine its success is how (or if) Amazon and Johnson brag about its viewership. Who knows if theres any hopes to turn this into a holiday franchise, but no doubt one or either parties would like this to be a win, even if its just being a reliable movie to have in holiday rotation for the next few years. Want more io9 news? Check out when to expect the latest Marvel, Star Wars, and Star Trek releases, whats next for the DC Universe on film and TV, and everything you need to know about the future of Doctor Who.0 Σχόλια 0 Μοιράστηκε 149 Views
GIZMODO.COMAmazons Fine With Red One Not Being a Box Office HitIts time for the holiday movie season, and Amazons kicking things off with its action-comedy feature Red One. The film has a lot of star power behind it, with Dwayne Johnson and Chris Evans playing an odd couple tasked with saving a kidnapped Santa Claus (J.K. Simmons), and its trailers have made it seem like it could be either surprisingly good or a complete mess. And the answer appears to be kind of both? Reaction-wise, audiences have taken toRed Onemuch more than critics, most of whom did not really care for it. Thats further reflected in its just okay box office: of the films $84.1 million box office, $34.1 million of that was domestic, and generally in line with its projected $30-35 million range. However, as noted by Variety, the movie itself reportedly cost a hefty $250 million to make, and its biggest accomplishment is halting Venom: The Last Dances continued domestic reign over the last few weeks. Time might not also be on Red Ones side, since its about to be a pretty crowded time at the movies between Wicked: Part I, Gladiator II,and Moana 2 So depending on your thinking, it might be curtains for Red Onestheatrical run in the near futurethough Amazon MGMs theatrical head isnt quite looking to throw in the towel just yet. Amidst those other movies, he believes the Christmas flick offers something a little different than those movies, but stopped short of saying what that something differentis. But even if the movies not a box office hit, the studios more confident itll land with audiences once it hits Prime Video, similar to how Aprils Road Houseremake was such a streaming hit to get a sequel greenlit. According to him, Amazon films getting theatrical runs can help cover the marketing costs ahead of streaming, which is reason enough to let them play on the big screen for a few weeks.WheneverRed Onehits Prime Video, the real way to determine its success is how (or if) Amazon and Johnson brag about its viewership. Who knows if theres any hopes to turn this into a holiday franchise, but no doubt one or either parties would like this to be a win, even if its just being a reliable movie to have in holiday rotation for the next few years. Want more io9 news? Check out when to expect the latest Marvel, Star Wars, and Star Trek releases, whats next for the DC Universe on film and TV, and everything you need to know about the future of Doctor Who.0 Σχόλια 0 Μοιράστηκε 149 Views



